Introduction
Many people type “adenoidid” when they’re searching for information about adenoiditis—a condition involving inflamed or infected adenoids. Adenoiditis is most common in children, but it can affect teens and adults too. Because adenoids sit high behind the nose, inflammation there can cause stubborn congestion, mouth breathing, snoring, bad breath, and even ear problems. This article explains adenoiditis from top to bottom—what it is, why it happens, what symptoms look like, how doctors diagnose it, what treatments are used, and when surgery is considered.
1) What are adenoids?
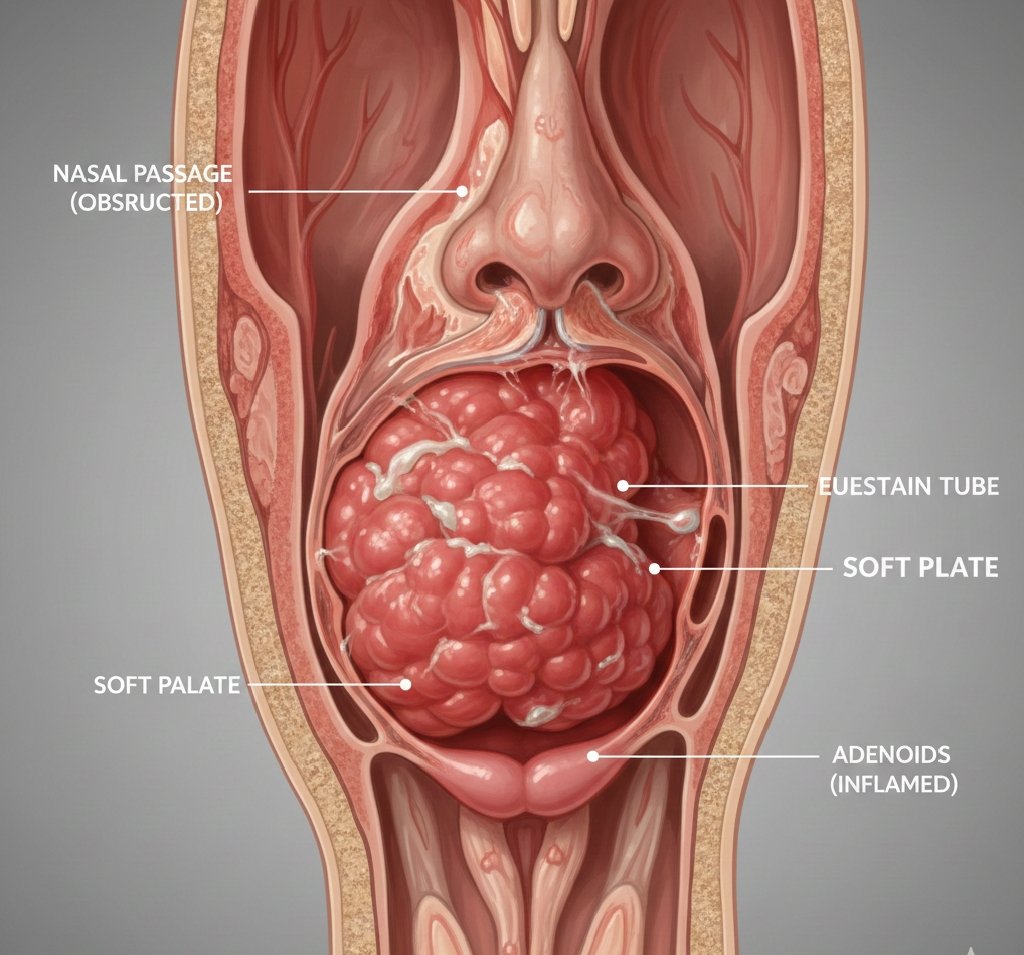
Adenoids are a patch of immune tissue located in the nasopharynx (the area behind the nose and above the back of the throat). Along with the tonsils, they are part of the body’s immune defense system. In young children especially, adenoids help “sample” germs that enter through the nose and mouth and support immune responses.
A key detail: adenoids naturally change with age. They’re generally largest in childhood and often shrink during adolescence. Because of this, adenoid problems are most discussed in pediatrics. Still, when adenoids become chronically inflamed, they can create significant symptoms—especially related to breathing and sleep.
2) What is adenoiditis?
Adenoiditis means inflammation of the adenoids. Often, it happens because of infection, but it can also be driven by chronic irritation such as allergies. Adenoiditis can be:
- Acute (short-term): inflammation during or after a cold or upper respiratory infection.
- Chronic (long-term): symptoms persist for weeks/months or keep returning, sometimes without fully clearing between episodes.
Adenoiditis is closely linked to adenoid hypertrophy, which means enlarged adenoids. Repeated inflammation can make adenoids swell and remain larger than normal, and enlarged adenoids can then worsen congestion and blockage—creating a cycle that keeps symptoms going.
3) Causes: why adenoids get inflamed
Adenoiditis is usually triggered by things that irritate or infect the upper airway:
A) Viral infections
Many cases start as a typical viral illness: runny nose, sore throat, mild fever, cough. Even after the virus improves, adenoids can remain swollen and irritated.
B) Bacterial infections
Sometimes bacteria contribute—especially when symptoms are prolonged, worsen after briefly improving, or involve thick nasal discharge and significant fever. Bacterial involvement may be more likely in chronic cases or when sinus infections are also present.
C) Allergies
Allergies can cause chronic inflammation and swelling throughout the nose and throat. When allergic inflammation affects the adenoids, symptoms may look like “constant congestion” rather than an obvious infection.
D) Irritants and environment
Secondhand smoke, air pollution, very dry air, and frequent exposure to respiratory infections (like in daycare or school) can worsen upper airway inflammation.
E) Reflux irritation
In some people, stomach acid reflux reaching the throat can irritate tissues in the upper airway and contribute to chronic inflammation.
4) Symptoms of adenoiditis
Symptoms depend on how swollen the adenoids are and whether infection is active. Common symptoms include:
Nasal and breathing symptoms
- Stuffy nose / blocked nasal breathing (often persistent)
- Mouth breathing, especially noticeable at night
- Nasal speech (a “stuffy” voice)
- Runny nose or chronic drainage
- Postnasal drip (mucus dripping down the throat)
Throat and general symptoms
- Sore throat (often from postnasal drip)
- Cough, especially at night
- Bad breath (halitosis)
- Low-grade fever (more common in acute infection)
- Swollen neck glands sometimes
Sleep-related symptoms
Because adenoids sit near the nasal airway, swelling can disrupt sleep:
- Snoring
- Restless sleep
- Frequent waking
- Daytime tiredness or irritability in children
- In more severe cases, signs of sleep apnea (pauses in breathing, gasping, choking sounds)
Ear-related symptoms (very common in children)
Adenoids are located near the opening of the Eustachian tubes, which help equalize pressure in the middle ear. When swollen, adenoids can interfere with that function:
- Ear fullness or pressure
- Middle ear fluid
- Frequent ear infections
- Temporary hearing difficulties
5) Why adenoiditis can look like “constant colds”
A common frustration for parents is that a child seems to have a “cold” all the time. That can happen when:
- the child catches frequent viruses, and the adenoids never fully calm down;
- allergies are causing constant inflammation;
- enlarged adenoids are creating chronic blockage and mucus buildup;
- the child snores and sleeps poorly, leading to fatigue and behavioral changes that feel like illness.
In those cases, the issue isn’t always “one infection that won’t go away”—it may be repeated triggers causing ongoing inflammation.
6) Diagnosis: how clinicians figure it out
Doctors usually diagnose adenoiditis using:
A) History and symptom pattern
They’ll ask how long symptoms last, whether they keep returning, how sleep is going, whether there are ear infections or hearing issues, and whether allergy symptoms are present.
B) Physical exam
A standard exam can’t easily “see” the adenoids directly because they sit behind the nose. But doctors can look for indirect clues: nasal congestion, mouth breathing, throat redness, postnasal drip, or enlarged lymph nodes.
C) ENT evaluation (if needed)
If symptoms are persistent, severe, or complicated (sleep apnea signs, repeated ear infections, failure of treatment), an ENT specialist may evaluate the nasopharynx more directly—often with a small flexible scope.
7) Treatment: what actually helps
Treatment depends on whether the main driver is viral inflammation, bacterial infection, allergies, reflux, or structural enlargement.
A) Supportive care (especially for mild/acute cases)
Many mild cases improve with time and symptom relief:
- fluids and rest
- saline nasal spray/rinses (age-appropriate)
- humidified air to reduce dryness
- fever/pain control as recommended by a clinician
B) Medications (when appropriate)
A clinician may recommend:
- Antibiotics if bacterial infection is suspected or symptoms are prolonged and severe
- Nasal steroid sprays to reduce inflammation, especially if allergies or chronic swelling are involved
- Allergy treatment (depending on the person), which may include avoiding triggers and using appropriate medications
- Reflux management if reflux seems to be contributing (this can include diet changes and clinician-guided therapy)
Important note: it’s common for families to try multiple approaches because symptoms may come from more than one cause. For example, a child might have mild allergies and frequent viruses, and both contribute to adenoid swelling.
C) When surgery is considered: adenoidectomy
If adenoiditis becomes chronic or adenoid enlargement causes major obstruction, doctors may recommend adenoidectomy (surgical removal of the adenoids). This is more likely if there is:
- significant nasal obstruction with persistent mouth breathing
- loud snoring or signs of sleep apnea
- repeated or ongoing symptoms despite appropriate medical treatment
- recurrent ear infections or persistent middle ear fluid, sometimes with hearing concerns
Adenoidectomy is common in children and is typically done through the mouth (no visible incision). Recovery is usually straightforward, though every surgical decision should be individualized.
8) Possible complications if the problem persists
Adenoiditis and chronically enlarged adenoids can contribute to:
- sleep disruption, leading to fatigue, irritability, and difficulty focusing
- recurrent ear infections or persistent middle ear fluid
- hearing issues (often temporary, but still important)
- chronic mouth breathing, which may lead to dry mouth, throat irritation, and dental issues over time
- worsening quality of life for the child and family due to poor sleep
9) When to seek urgent care
Seek urgent medical help if there is:
- difficulty breathing, struggling to get air, or bluish lips
- suspected severe sleep apnea with frequent pauses/gasping
- dehydration (especially in children)
- high fever with worsening lethargy, severe neck stiffness, or rapidly worsening symptoms
10) Practical prevention and home habits
You can’t prevent every respiratory infection, but you can reduce triggers:
- encourage good hand hygiene
- keep indoor air comfortably humid (not overly dry)
- reduce smoke exposure (including secondhand smoke)
- manage allergies if they’re suspected
- keep a symptom diary: snoring frequency, sleep quality, number of infections, ear symptoms—this helps clinicians make faster, more accurate decisions
Conclusion
Adenoiditis is inflammation of the adenoids that commonly affects children and can cause persistent congestion, mouth breathing, snoring, postnasal drip, cough, bad breath, and ear problems. Many cases are mild and improve with supportive care, but chronic or severe symptoms deserve medical evaluation—especially when sleep is disrupted or ear infections are frequent. Treatment ranges from symptom relief and anti-inflammatory approaches to antibiotics when appropriate, and in selected cases, adenoidectomy can provide major relief. The key is recognizing patterns: if symptoms are persistent, recurrent, or affecting sleep and hearing, it’s worth getting a clinician—often an ENT—to take a closer look.